habits of the household study guide

Household Study Guide: Cultivating Effective Habits
Establishing consistent routines is key to a well-maintained home, fostering peace and reducing stress. Daily habits, like quick tidy-ups and immediate dishwashing, dramatically improve efficiency.
Leveraging habit stacking and dedicated cleaning days further streamlines chores. Minimizing clutter through regular purging and utilizing vertical storage maximizes space and simplifies upkeep.
The Importance of Daily Cleaning Routines
Daily cleaning routines are the cornerstone of a consistently tidy and comfortable home environment. They shift the focus from overwhelming, infrequent deep cleans to manageable, bite-sized tasks integrated seamlessly into your everyday life. This proactive approach prevents clutter from accumulating and becoming a daunting challenge.
A little effort each day yields significant long-term benefits. Consider the impact of a quick 15-minute tidy-up session – it prevents surfaces from becoming overrun and maintains a sense of order. Similarly, immediately washing dishes after meals avoids the buildup of dirty dishes in the sink, a common source of household stress.

These routines aren’t about striving for perfection, but about maintaining a baseline level of cleanliness. It’s about establishing habits that become second nature, requiring minimal conscious effort. This frees up valuable time and energy for more enjoyable pursuits, contributing to a more relaxed and harmonious household. Consistent daily routines are a powerful tool for cultivating a peaceful and organized living space.

15-Minute Tidy-Up Sessions
Integrating 15-minute tidy-up sessions into your daily schedule is a remarkably effective strategy for maintaining a consistently organized home. These short bursts of focused effort prevent clutter from spiraling out of control, making cleaning feel less overwhelming and more achievable.
The key is to concentrate on one area at a time. Perhaps focus on the living room, kitchen counters, or a specific bedroom. Set a timer for 15 minutes and dedicate yourself solely to tidying that space – putting things away, wiping surfaces, and generally restoring order.
Don’t get bogged down in deep cleaning during these sessions. The goal is quick wins and visible improvements. Focus on surface-level organization and immediate decluttering. These sessions are about progress, not perfection.
Consistency is crucial. Even a few 15-minute sessions each week can dramatically impact the overall cleanliness and order of your home. Make it a habit, and you’ll find that maintaining a tidy space becomes significantly easier and less stressful.

Making Your Bed Every Morning
Starting your day by making your bed is a surprisingly powerful habit with far-reaching benefits beyond just a tidy bedroom. It’s a small accomplishment that sets a positive tone for the entire day, fostering a sense of order and control from the moment you wake up.
This simple act provides an immediate sense of accomplishment. Completing this task first thing creates momentum, making you more likely to tackle other responsibilities with enthusiasm. It’s a psychological boost that can improve productivity throughout the day.
A made bed also contributes to a more peaceful and inviting bedroom environment. It visually declutters the space, reducing stress and promoting relaxation. Returning to a neatly made bed at the end of the day offers a sense of calm and comfort.
Don’t overthink it; simplicity is key. A quick straightening of the sheets and fluffing of pillows is sufficient. Make it a non-negotiable part of your morning routine, and experience the positive ripple effect it has on your overall well-being and household organization.
One-Touch Rule for Clutter
The “One-Touch Rule” is a remarkably effective strategy for minimizing clutter and maintaining a tidy home. It’s based on the principle that you should only handle an item once – deal with it immediately instead of putting it down to address later.
This means that when you pick something up, you immediately decide what to do with it: put it away, file it, donate it, or discard it. Avoid creating piles of “to-do” items or temporary holding zones. These quickly escalate into overwhelming clutter.
Applying this rule prevents items from migrating around the house and accumulating in unwanted areas. It forces you to make a decision upfront, eliminating the mental energy wasted on repeatedly handling the same objects.
Start small, focusing on frequently used items. As you become more accustomed to the rule, expand its application to all areas of your home. Consistent implementation of the One-Touch Rule dramatically reduces clutter build-up and fosters a more organized and peaceful living space.
Immediate Dishwashing After Meals
Establishing a habit of immediate dishwashing after meals is a cornerstone of a consistently clean kitchen and a more relaxed household. Letting dishes pile up creates a daunting task and can quickly lead to a chaotic environment.
The key is to tackle the dishes while food remnants are still fresh and easier to remove. This prevents food from drying and hardening, reducing scrubbing time and effort. Even a quick rinse and stack can make a significant difference if a full wash isn’t immediately feasible.
Consider it a part of the mealtime routine – once everyone is finished eating, the dishes are addressed. This prevents the task from being postponed and forgotten. Involving all household members in this habit fosters a sense of shared responsibility.
A clean kitchen promotes a sense of calm and order, making it a more inviting space. By consistently washing dishes immediately, you avoid the stress of a looming pile-up and maintain a hygienic environment. It’s a small habit with a substantial positive impact.
Laundry Schedule: Preventing Overwhelm
A well-defined laundry schedule is crucial for preventing mountains of dirty clothes and the associated stress. Letting laundry accumulate leads to a feeling of being constantly behind and can quickly become overwhelming.
Instead of tackling laundry as a massive, infrequent chore, break it down into smaller, manageable loads throughout the week. Assign specific days for different types of laundry – for example, whites on Monday, colors on Wednesday, and towels on Friday.
Consider the needs of your household and adjust the schedule accordingly. Families with children may require more frequent laundry days. Involving all household members in sorting and folding can lighten the load for everyone.
Sticking to a schedule creates a sense of control and predictability. It ensures that laundry is consistently addressed, preventing it from spiraling out of hand. A consistent routine minimizes the mental burden of constantly thinking about laundry. This frees up time and energy for other tasks and activities, contributing to a more balanced and peaceful home life;
Dedicated Cleaning Days for Specific Zones
Instead of attempting to clean the entire house at once, a more effective approach is to dedicate specific days to particular zones. This method breaks down a daunting task into smaller, more achievable segments, preventing burnout and fostering a sense of accomplishment.
For example, Monday could be for bathrooms, Tuesday for kitchens, Wednesday for bedrooms, and Thursday for living areas. This allows for focused attention and a more thorough cleaning of each space.
Within each zone, create a checklist of tasks to ensure consistency. This might include wiping down surfaces, vacuuming or mopping floors, and cleaning appliances. Remember to declutter before cleaning to maximize efficiency.
This zoned approach also allows for deeper cleaning tasks to be incorporated on a rotating basis. For instance, cleaning out the refrigerator could be a monthly kitchen task. By spreading out the workload, maintaining a clean and organized home becomes less overwhelming and more sustainable. This contributes to a more peaceful and enjoyable living environment.
Decluttering as a Regular Habit
Decluttering isn’t a one-time event; it’s an ongoing process crucial for maintaining a tidy and functional home. Integrating decluttering into your routine prevents accumulation and makes cleaning significantly easier. A key principle is to regularly purge unused items, questioning whether they bring value or joy.
Implement a “one-in, one-out” rule: for every new item brought into the house, an old one must be discarded. This prevents clutter from spiraling out of control. Schedule short, frequent decluttering sessions – even 15 minutes a day can make a substantial difference.
Focus on one area at a time, such as a drawer, shelf, or corner. Donate, sell, or discard items you no longer need or use. Be ruthless in your assessment, considering practicality and emotional attachment. Regular decluttering minimizes purchases, reducing the overall cleaning burden and fostering a more minimalist lifestyle.
A clutter-free home promotes a sense of calm and order, contributing to a more peaceful and productive environment. It’s a habit that yields long-term benefits for both your physical space and mental well-being.
Utilizing Vertical Space for Storage
Maximizing vertical space is a game-changer for smaller homes or those prone to clutter. It transforms unused areas into valuable storage solutions, creating a more organized and spacious environment. Think beyond floor-level storage; walls are your allies!

Install shelves – floating shelves, bookcases, or wall-mounted units – to store books, décor, and everyday items. Utilize tall, narrow cabinets to fit into tight spaces. Over-the-door organizers are excellent for pantries, bathrooms, and closets, holding shoes, toiletries, or cleaning supplies.
Hooks are incredibly versatile; use them for coats, bags, towels, or even pots and pans in the kitchen. Consider stacking storage containers vertically, maximizing space in cupboards and closets. Don’t forget the space above furniture! Add shelves above sofas or beds for additional storage.
Effective vertical storage reduces floor clutter, making rooms feel larger and more open. It’s a practical and aesthetically pleasing way to enhance organization and streamline your household routines.
The Power of Habit Stacking
Habit stacking is a powerful technique for building new routines by linking them to existing ones. Instead of trying to overhaul your entire cleaning schedule at once, integrate small cleaning tasks into habits you already perform daily. This leverages the momentum of established behaviors, making new habits stickier.
For example, after you brush your teeth each morning, wipe down the bathroom counter. Or, while your coffee brews, unload the dishwasher. After you sit down to watch TV, fold a load of laundry. These small additions, when consistently performed, accumulate into significant cleaning progress.
The key is to choose existing habits that are reliable and frequent. The new habit should be simple and easy to accomplish immediately after the trigger habit. Start small and gradually increase the complexity as the habit becomes ingrained.
Habit stacking minimizes willpower depletion and makes cleaning feel less daunting. It transforms chores from isolated tasks into natural extensions of your daily routine, fostering a consistently cleaner home.
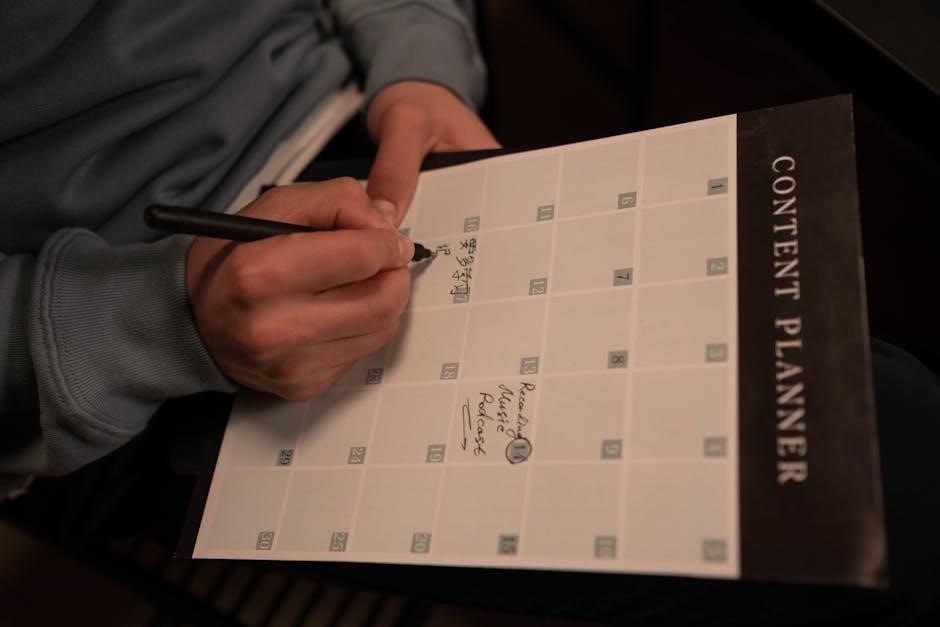
Creating a Cleaning Checklist

A well-structured cleaning checklist is the cornerstone of a consistent cleaning routine. It provides a clear roadmap, ensuring no task is overlooked and promoting a sense of accomplishment as items are checked off. The checklist should be tailored to your household’s specific needs and lifestyle.
Break down cleaning tasks into manageable steps. Instead of “Clean the bathroom,” list “Clean the toilet,” “Wipe down the sink,” and “Mop the floor.” Categorize tasks by frequency – daily, weekly, monthly, or seasonal. Daily tasks might include making the bed and wiping kitchen counters, while monthly tasks could involve deep cleaning appliances.
Consider using a digital checklist app or a simple paper list. Digital apps offer features like reminders and progress tracking. Involve all household members in creating the checklist to foster shared responsibility.
Regularly review and update the checklist as your needs evolve. A dynamic checklist ensures it remains relevant and effective in maintaining a clean and organized home.
Involving All Household Members
Shared responsibility is paramount for sustainable household cleanliness. Assigning age-appropriate chores to each member fosters a sense of ownership and teamwork, preventing one person from bearing the entire burden. Open communication is crucial when distributing tasks; consider individual schedules and capabilities.
Start with simple assignments for younger children, like putting away toys or setting the table. As they grow, gradually introduce more complex tasks. For teenagers and adults, clearly define expectations and provide necessary instructions. A rotating chore chart can ensure fairness and prevent monotony.
Frame chores not as punishments, but as contributions to a shared living space. Positive reinforcement and appreciation can motivate participation. Celebrate collective achievements, like completing a weekly cleaning schedule.
Lead by example; demonstrate a proactive attitude towards cleaning. When everyone contributes, maintaining a clean and organized home becomes a collaborative effort, fostering a more harmonious living environment.
The Role of Music and Motivation
Transforming chores from drudgery into enjoyable activities is achievable with the right mindset and tools. Music serves as a powerful motivator, injecting energy and rhythm into cleaning routines. Create upbeat playlists tailored to different tasks – energetic tracks for quick tidying, calming melodies for detailed cleaning.
Beyond music, gamification can enhance motivation. Set timers and challenge yourself to complete tasks within a specific timeframe. Reward yourself after achieving cleaning milestones, fostering a positive association with housework.
Visual cues and reminders also play a vital role. A cleaning checklist prominently displayed serves as a constant prompt. Break down large tasks into smaller, manageable steps to avoid feeling overwhelmed.
Cultivate a positive attitude towards cleaning. Focus on the benefits – a clean home promotes relaxation, reduces stress, and enhances overall well-being. Remember, a little effort each day prevents a massive cleaning overhaul later on.
Minimizing Purchases to Reduce Cleaning
A fundamental aspect of simplifying housework lies in conscious consumption. Each new item introduced into the home inevitably requires cleaning, organizing, and potential maintenance. Adopting a minimalist approach, focusing on needs rather than wants, significantly reduces the overall cleaning burden.

Before making a purchase, consider its necessity and potential impact on your cleaning routine. Ask yourself if the item truly adds value to your life or if it will simply contribute to clutter. Prioritize quality over quantity, investing in durable, long-lasting items that require less frequent replacement.
Embrace the concept of “one in, one out.” For every new item you acquire, commit to donating or discarding a similar item. This prevents accumulation and maintains a manageable level of possessions.
Resist impulse buys and marketing tactics. Take time to research products and compare prices before making a decision. A thoughtful approach to purchasing translates directly into a cleaner, more organized, and less stressful home environment.
Regularly Purging Unused Items
Decluttering isn’t a one-time event; it’s an ongoing process vital for maintaining a manageable home. Items accumulate over time, often becoming unused and occupying valuable space. Regularly purging these items creates a lighter, more organized living environment, directly reducing cleaning demands.
Schedule dedicated purging sessions – quarterly or even monthly – to systematically review belongings. Focus on areas prone to clutter, such as closets, drawers, and storage spaces. Be ruthless in your assessment: if an item hasn’t been used in six months to a year, seriously consider letting it go.
Employ the four-box method: keep, donate, discard, and relocate. This provides a clear framework for decision-making. Donating usable items extends their life and benefits others, while discarding broken or unusable items frees up space.
Remember the emotional attachment to possessions can hinder the process. Ask yourself if the item brings joy or serves a practical purpose. If not, release it. A clutter-free home fosters a sense of calm and control, making cleaning significantly easier.

Reward System for Maintaining Habits
Sustaining new habits requires positive reinforcement. A reward system acknowledges effort and motivates continued adherence to cleaning routines. It transforms chores from burdensome tasks into achievements worthy of celebration, fostering a more positive association with housework.

Rewards don’t need to be extravagant; they should be meaningful and aligned with personal preferences. Small treats, like a relaxing bath, an evening with a good book, or a favorite snack, can be highly effective. For larger milestones, consider a family outing or a small purchase.
Implement a tiered system: daily rewards for completing daily tasks, weekly rewards for consistent adherence to the schedule, and monthly rewards for significant achievements. This provides ongoing motivation and acknowledges progress at different levels.
Involve all household members in designing the reward system, ensuring it’s fair and appealing to everyone. Visual trackers, like charts or calendars, can provide a sense of accomplishment and reinforce positive behavior. Acknowledging and celebrating successes is crucial for long-term habit formation.